A new paradigm for exoprostheses – 3D printing in prosthetics

Even though it is undoubtedly a last resort, amputations are not uncommon in Germany either. According to the latest publicly available data from 2021, the number of amputations on upper and lower extremities in Germany was 65,464.
The number of major amputations, i.e. amputations proximal to the ankle or wrist, is steadily decreasing, but is still higher than the number of minor amputations, i.e. amputations distal to the ankle or wrist.
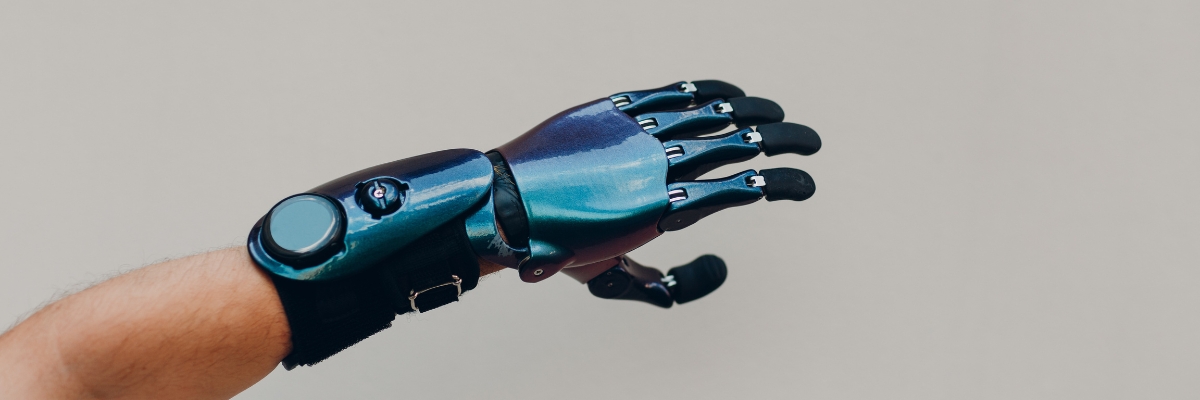
In particular, exoprostheses are often essential for these major amputations to enable people to get their lives back on track. Prostheses must fulfil many different requirements, including individual adaptation to the patient's residual limb, a high degree of comfort, antibacterial properties and much more.
Combining all these properties using conventional methods is possible, but costly. Even prostheses for minor amputations cost several thousand euros, and full prostheses can quickly reach five figures.
However, 3D printing opens up a new paradigm for exoprosthetics. In this blog post, I would like to introduce this paradigm and thus explain the advantages that 3D printing offers in prosthetics.

The conventional process and its bottlenecks
To fully grasp the advantages of 3D printing, it is first essential to understand the conventional process for manufacturing exoprostheses, at least in broad terms, and thus to evaluate its bottlenecks.
In both processes, the focus is initially on manufacturing the prosthesis socket. In the traditional process, an orthopaedic technician begins by thoroughly examining the residual limb. By examining and measuring it, the orthopaedic technician gains an overview of the skin condition, volume and bony prominences of the amputation stump.
The orthopaedic technician then makes a negative plaster cast of the stump. To do this, plaster bandages are wrapped around either the residual limb or the prosthesis liner and, once the plaster has set, these bandages are carefully removed. This negative mould is then filled with plaster to create a solid, three-dimensional replica of the residual limb, which is used to create the prosthesis socket.
However, before the socket can be created, the prosthetist needs to make some adjustments to the positive model. This involves adding material to areas that require additional volume, particularly bony areas, and removing material from weight-bearing areas.
Using this modified residual limb replica, a test socket is now produced using traditional manufacturing methods, a process that takes between three and six weeks. Once the test socket is completed, the patient is asked to wear it and perform some basic movements with it. This allows the prosthetist to assess potential pressure points where the socket needs to be widened or additional padding added, as well as the dynamic alignment of the socket during movement.
Minor adjustments, such as adding or removing padding, can be made directly, but major adjustments, such as remodelling, require the test socket to be remade. On average, this iterative fitting process takes between 7 and 18 visits by the patient, depending on the complexity, and about 16 remakes of the test socket.
After the fitting process is complete, the final prosthetic socket is produced based on the last test socket. This is used to carry out a final round of tests to confirm the perfect fit, whereupon the first essential part of the exoprosthesis is ready.
The other components of the prosthesis, including joints and suspension systems, must also be carefully selected or manufactured. Here, too, individuality plays a major role, but not quite as much as with the socket, which means that the number of patient visits and new productions of these components is usually lower.
Traditional manufacturing systems excel in many areas, but when it comes to customisation, they quickly reach their limits. Lead times, changeover times and the amount of work involved increase massively due to the constant need to adapt the socket and the other components, thus not only extending the time a patient has to wait for a prosthesis, but also the costs.
The high degree of manual work also potentially increases the risk of human error. Such errors can lead to further waiting times and costs if, for example, an error has already crept in during the creation of the plaster cast of the residual limb – and even very small inaccuracies can be enough to cause this.
The digital process and its advantages
Although the digital process has 3D printing at its core, a 3D printer cannot, of course, do all the work of a medical professional – but it can make a massive contribution to reducing it.
Here, too, the orthopaedic technician begins by examining and documenting the residual limb. Once he has gained an overview of the stump's characteristics, imaging techniques are used to create a digital 3D model of the stump. With the right software, 2D images from an MRI, for example, can also be transformed into a three-dimensional image, but small 3D scanners are often used to scan the stump from all sides and angles.
The adjustments that the orthopaedic technician made to the plaster cast in the traditional process can now be made digitally much more easily and, above all, quickly. Using advanced software solutions, the model can even be used to carry out initial tests in terms of pressure points and dynamic alignment, and any necessary adjustments can be applied automatically.
Once the digital model is complete, it only needs to be exported in a suitable format and printing of the first test prosthetic socket can begin. Both filament and resin 3D printing are suitable as the technology of choice, with resin and powder 3D printing being particularly suitable due to their outstanding precision.
Depending on the printing technology, the printing process for the prosthetic socket can be completed in just a few hours or a day. The socket then needs to be reworked using different methods depending on the technology used. Chemical vapour smoothing, in particular, has established itself as the ideal reworking tool due to its ability to improve surface smoothness and seal potential porosities. On average, a patient can expect a waiting time of only a few days before the first tests are carried out using the digital process.
Of course, these tests are also of the utmost importance in the digital process. According to several studies, including this one, significantly better results can be achieved by using software that digitally simulates the first tests, which means that the number of iterations can be reduced later on.
The further process of prosthesis production is relatively similar. However, adaptations can be made much faster due to the existence of a digital model, which can be adapted with just a few clicks. Factors such as long lead or changeover times can be completely eliminated from the vocabulary when using 3D printing.
As soon as the perfect fit for the socket has been found, the final socket can be produced. While 3D printing did not have the necessary materials to produce durable and functional exoprostheses for a long time, this is now easily possible thanks to carbon fibre-reinforced materials, for example. Nevertheless, both processes can also be combined to continue producing the final prosthesis using established conventional methods – this also applies to the other necessary components.
The biggest advantage of the digital process is obvious – time saved. Instead of having to wait weeks for new test sockets, this process only takes a few days. This means that waiting times for prostheses can be reduced many times over, enabling patients to be fitted with a prosthesis much more quickly, especially in developing countries.
Another major advantage concerns the digital model itself. Its availability makes it much easier to carry out not only adjustments for initial prostheses, but also subsequent adjustments that may be necessary over time due to changes in the volume of the residual limb, for example.

Why isn't 3D printing the standard yet?
I am almost reveling in the advantages of 3D printing here, but in the vast majority of hospitals, medical care centres and practices, traditional methods are still used to manufacture prostheses. Before we come to some case studies in which 3D printing has already been successfully used for exoprostheses, I would like to briefly discuss these factors.
The first factor is relatively easy to quantify – initial costs. However, this is not because 3D printers are necessarily more expensive than conventional prosthesis manufacturing equipment, but because the traditional machines are already in place. Switching to a new technology requires new investment, which often poses a significant challenge, especially for small to medium-sized healthcare providers.
The second and probably even more important factor is the potential lack of expertise in 3D printing. The use of 3D printing for prostheses is still comparatively new, which is why trained medical professionals are much rarer.
To solve this problem, many small to medium-sized healthcare providers rely on 3D printing service providers, who can use their expertise to support them in particular in the production of test sockets for prostheses, thus providing the advantages of 3D printing without the need for large initial investments.
If you need a suitable service provider to support you in 3D printing, from the initial idea to realisation, you can find more information here.

Case studies of 3D-printed exoprostheses
There are now a large number of case studies for 3D printing of exoprostheses, of which I would like to present two particularly interesting ones here, whereby I will always link to the complete case study or website.
An inspiring example includes Ben Ryan and his son Sol from the UK. There were complications during the birth of Sol, which led to a blood clot in Sol's left arm. To prevent further complications, the doctors were forced to amputate the arm just below the elbow.
Ben, who is actually a psychology lecturer, immediately started looking for suitable prostheses for his child, but according to NHS (National Health Service) guidelines, Sol would have had to wait a year for a cosmetic prosthesis and as long as three years for a functional prosthesis. However, various studies show that a child who receives an artificial limb earlier is far less likely to reject it. The earlier a functional prosthesis is fitted, the more likely it is that a child will use it into adulthood.
Ben taught himself how to make an exoprosthesis for his son, initially using very simple methods but later with 3D printing. With a Stratasys® 3D printer, Ben was able to print a prosthesis prototype for his son in just five days and also used 3D printing for the final prosthesis for a number of key elements.
Ben has since set up his own business using the knowledge he taught himself. Ambionics, a non-profit organisation, was born out of Ben's drive coupled with the skills of 3D printing, which Ben continues to use as his main tool to this day to help children in particular to receive prostheses as early as possible, continuing to use 3D printing as his main tool. The full case study can be found here.
The second example is about Easton LaChapelle, who founded Unlimited Tomorrow at the age of 17 to make 3D-printed prostheses available to everyone at a low cost.
Even as a teenager, Easton was fascinated by robotics and prosthetics. He was particularly inspired when he met a girl at a research fair who was wearing a prosthetic arm. This prosthesis had only one sensor and could only perform one movement – open and closed – but nonetheless cost $80,000.
Easton began tinkering in his bedroom. Using Lego bricks, fish hooks and small motors, he set about developing a robotic hand – and succeeded, at just 14 years old.
Today, 3D printing is the key piece of equipment for Easton and his company. It allows the company to create fully functional, custom-fit prostheses in just eight weeks – a process that can take over a dozen months using conventional methods. Visit the Unlimited Tomorrow website here.

Conclusion
While 3D printing has long been used exclusively as an aid in prosthetics, it has now become an all-purpose weapon. Whether pure shaft prototypes or complete exoprostheses – 3D printing enables a significantly faster and more cost-efficient manufacturing process for exoprostheses, which helps both medical professionals and patients.
However, 3D printing is still a long way from reaching its full potential. With constant research into new materials and technologies, this technology will continue to develop in this area, leading to ever better results.
If you want to stay up to date with the latest developments in 3D printing for prosthetics, please check this blog often – I will always post the latest developments here as soon as possible.
Thank you for your attention – and see you in the next blog post!






