The fight against breast cancer – how 3D Printing helps

Breast cancer is one of the most widespread types of cancer worldwide. According to the World Cancer Research Fund, almost 2.3 million new cases of breast cancer were detected in women in 2022, including over 74,000 in Germany. In the same year, over 666,000 women worldwide died from breast cancer.
This makes breast cancer the fourth most common fatal form of cancer, after hepatocellular carcinoma (liver cancer), colorectal carcinoma (bowel cancer) and bronchial carcinoma (lung cancer). And even if many men are unaware of it, they can also suffer from breast cancer. Although the proportion of men with breast cancer is less than 1% in contrast to women, the mortality rate is according to a study from the United States 19% higher than that of women – especially due to breast cancers being detected too late.
Breast cancer screening is of fundamental importance when it comes to preventing deaths. Breast cancer is considered to be one of the comparatively more treatable types of cancer, which is supported by the five-year survival rate of about 90% for breast carcinomas detected in the early stages. You can find more information about breast cancer prevention here.
As with all types of cancer, time is often of the essence when it comes to breast cancer. Rapid detection and treatment of breast cancer is the most important tool for keeping the chances of survival high.
This blog post is about how 3D printing can help medical centres, doctors and surgeons to speed up breast cancer detection and improve treatment.

Education and Training
Medical education and training plays an essential role in the detection of breast cancer. No matter how advanced the technologies for detecting breast cancer become, they will not be effective without trained physicians to use them or recognise early warning signs.
One of the most common procedures for detecting breast cancer is core needle biopsy. In this minimally invasive diagnostic procedure, a biopsy needle is inserted into the breast tissue under imaging guidance, for example ultrasound, and a cylindrical sample of the suspicious tissue is taken, which is then clinically analysed.
This method, which is far less invasive than a classic surgical biopsy, requires a very high degree of precision. In addition to physical practice, universal breast models made of silicone, gelatine or latex are often used, which are usually produced using various casting methods.
However, these conventional models come with some difficulties. On the one hand, they are relatively expensive; depending on the complexity, realistic breast models cost between 500 and 2,000 euros each. On the other hand, the uniformity of the models offers less practical experience, since in reality every breast and every tumour has individual characteristics.
3D printing supports medical colleges and universities in this regard by enabling them to produce a range of breast models quickly and cost-effectively. This allows trainee and qualified surgeons to practice on more rare clinical cases.
But what about precision, which is undoubtedly the most important factor in core needle biopsy, and which of course is also of the utmost importance in practice? Creighton University in Omaha, Nebraska, has used the multi-material capabilities of the Stratasys® Digital Anatomy platform to create breast models for training core needle biopsies and was more than thrilled with the results.
Together with a radiologist specialising in breast diagnostics, they found that the 3D-printed model even allowed for more precision than conventional silicone models. With prefabricated silicone models, the radiologist had found that the needle was pulled back unnaturally when inserted for the first time, which did not happen with the 3D-printed model. In addition, the biopsy well was closer to reality in the additively manufactured model than in the silicone models.
A different study from 2020 specifically addressed the anatomical accuracy of 3D-printed models as opposed to gelatin models. The 3D-printed models also achieved excellent results in this aspect, although there were difficulties with the ultrasound examination. Creighton University also experienced these difficulties at the beginning, but was able to overcome them after making some minor adjustments to the ultrasound machine, thus enabling the 3D-printed models to be used to their full extent.
All in all, 3D printing enables medical education and training institutions to produce anatomically more accurate, cost-effective and customised breast models that make training in essential examinations, particularly core needle biopsies, more realistic.

Preoperative Planning
Once a patient has been diagnosed with breast cancer, time is of the essence. In order to prevent an increase in size or even a metastasis, surgery to remove the tumour completely, which is necessary in most cases, must be performed as quickly as possible to prevent an increase in size or even a metastasis.
This short time frame is made even more urgent by the fact that breast cancer treatment requires multidisciplinary collaboration between different fields such as surgery, oncology, pathology and radiology.
Nevertheless, extensive preoperative planning is of course also essential, regardless of whether breast-conserving surgery or mastectomy is to be performed. Insufficient preparation can lead not only to complications during the operation, but also afterwards, for example if positive resection margins (cut edges with tumour cells) have not been removed.
Traditionally, preoperative planning is carried out using 2D mammography or digital 3D MRI images. However, no matter how high the resolution, these images can never show the anatomical relationships between the tumour, the overlying skin, the mammary glands, the fatty tissue, the nipple and the pectoralis major muscle to the same extent as a real 3D object could.
To support surgeons in preoperative planning, the 3D files created by MRI can be converted into a suitable format and then transformed into a real 3D object using a 3D printer. Critical structures, such as blood vessels or lymph nodes, can be highlighted to develop a precise surgical strategy and minimise the invasiveness of the operation.
Furthermore, these models can support doctor-patient communication. Surgeons can use the model to describe to their patients in detail how exactly the operation will be performed and how they will ensure that it is safe. This not only gives patients a better understanding of their treatment, but also increases their sense of security.
Last but not least, these models can also be used to simulate surgery. Using realistic materials, such as Stratasys® DAP materials, the surgeon can perform the operation on the 3D printed model, receiving realistic tactile feedback.
3D printing and its possibilities represent a revolutionary advancement for preoperative planning. The realism that is now possible with 3D printing gives all parties involved a better understanding of the surgery and treatment of breast cancer.

Intraoperative Markings
But 3D printing is not only an ideal tool to facilitate the work of surgeons before an operation – it can also provide significant support during the operation.
In breast cancer surgery, previously taken 2D images are usually used for precise localisation. Wire or clips are also often used to mark the tumour on the breast during surgery. However, this method of intraoperative localisation leads to positive margins and thus to re-sections or even a recurrence in 20 to 30 per cent of cases.
3D printing offers the possibility of producing individual and exact surgical templates based on 3D data generated by imaging techniques. In the case of breast cancer surgery, these enable exact marking of the tumour on the breast, for example by injecting a blue dye.
A study from 2017 confirmed the success of such 3D-printed templates. The 3D-printed template was evaluated in 19 women with palpable breast cancer and was able to precisely localise 18 tumours, with all 68 injections with the blue dye being outside the tumour margins.
Another study involving over 400 subjects and investigating 3D-printed templates for tumour marking has been ongoing since 2020. Unfortunately, the results of this study are not expected until April of this year. However, with a success rate of almost 95% in the first study, we can undoubtedly look forward to these results with great interest.
By enabling more precise marking during breast surgery, 3D printing could in future be able to minimise positive margins and thus recurrent cancer, helping hundreds of thousands of women worldwide to leave cancer behind them for good.

Breast Reconstruction
After a mastectomy, breast reconstruction is an important final step in helping patients to return to their old lives. Studies, such as this Australian study from 2016, show that women who have a breast reconstruction after a mastectomy have a better psychosocial adjustment and a higher quality of life than women who do not have a breast reconstruction.
The most common type of breast reconstruction is implant-based breast reconstruction. However, autologous breast reconstruction, in which the breast is reconstructed using the body's own tissue flaps, has now developed into a better option, among other things by creating a more natural-looking breast and an even higher quality of life than with implant-based reconstructions, as this German study from 2022 has shown.
In autologous breast reconstruction, there are several sites from which tissue can be harvested for reconstruction. The DIEP flap (Deep Inferior Epigastric artery Perforator), an ellipsoidal lower abdominal fat flap that achieves a large flap mass and dimension, is used particularly frequently.
The success of this reconstruction is intrinsically linked to the identification and preparation of suitable vessels. However, since the vessels on the DIEP flap often take a complex path through the rectus abdominis muscle, intramuscular dissection is relatively time-consuming and conventional 2D methods for visualising the abdominal vascular anatomy, such as computed tomography angiography (CTA), only reveal the location of the perforators without clearly showing the complex course of intramuscular vessels.
The ability to turn these 2D models into real 3D objects provides surgeons with new options for realistically reconstructing the vascular system. As early as 2019, a collaboration between several medical universities used a combination of CTA scans, DICOM to print software and Stratasys® PolyJet™ technology, along with its multi-colour capabilities, to create models that accurately and clearly show the course of the vessels through the rectus abdominis muscle.
In addition to the level of detail, the outstanding print speed was particularly impressive. After the CTA scan was performed, the 3D and Quantitative Imaging team needed only between 48 and 72 hours to create a realistic 3D object from the 2D image and print it.
3D printing thus makes autologous breast reconstruction much safer. The more accurate representation of intramuscular vessels allows surgeons to better plan the removal, which can also increase the success rate of these breast reconstructions.
Bioprinting
While all the 3D printing options for fighting breast cancer discussed so far are already possible, the final section offers a glimpse into a possible future.
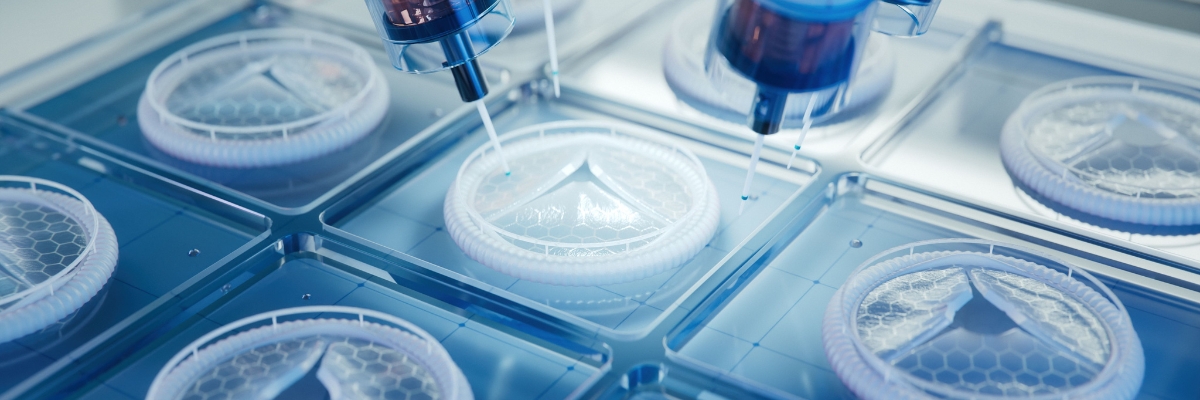
Bioprinting, the three-dimensional printing of biological tissue from living cells, has been actively researched since the 2000s. In particular, a considerable amount of progress has been made in this field in the 2010s – from 3D-printed skin and cartilage structures to mini-organs for testing new drugs.
This sci-fi-like technology could also be of great use in the future for breast cancer treatment, specifically breast reconstruction. Instead of a simple implant or taken autologous tissue, bioprinting could be used to print implants from the woman's own natural breast tissue.
While this scenario may still seem a long way off, a large number of studies are already being conducted on the bioprinting of breast tissue, for example this study, which has been running since 2023, or this study, conducted in 2018, which specifically deals with the reconstruction of the nipple-areola complex using 3D printing.
Only the future will tell whether bioprinting has the potential to fundamentally change medicine. However, the constant progress and study results give reason for hope. As soon as there are further developments in this area, you are sure to find the latest updates on this blog.

Conclusion
3D printing offers a wide range of extraordinary possibilities for combating breast cancer – including in the perioperative setting. From education and training to preoperative planning, intraoperative marking and breast reconstruction, advances in medical 3D printing are already enabling healthcare professionals around the world to provide better patient care.
As 3D printing continues to evolve, new possibilities are constantly emerging to further improve patient care. It will be exciting to see what advances the future holds – and how this technology can continue to help fight breast cancer more effectively.
Thank you for reading – and see you in the next blog post!






